Root canal treatment is a general dental procedure to save a badly infected or damaged tooth rather than pulling it out. During a root canal, the dentist removes inflamed or infected pulp (the soft tissue inside a tooth), cleans and disinfects the canals, then fills and seals them.
Despite its reputation, a modern root canal is usually no more painful than a typical filling, thanks to effective local anesthesia. In fact, after a root canal you often feel better than before, because the source of the tooth pain (the infection) has been eliminated.
In this article, you’ll learn what a root canal is and why you may need one, how long it takes, step-by-step treatment details, what level of pain or discomfort is normal afterward, and how to manage recovery. We’ll also cover how to prevent the need for a root canal and why delaying treatment can make problems worse. By the end, you’ll understand the process and know when to seek help.
What Is a Root Canal and Why Might You Need One?
Root canals are often misunderstood. Unlike old myths, the dentist is not drilling a “canal” into your jaw. The term simply refers to the canal of tissue inside the tooth. In reality, the procedure is straightforward. The dentist removes the existing pulp, cleans and disinfects the canal spaces, and then seals them.
Definition and Purpose
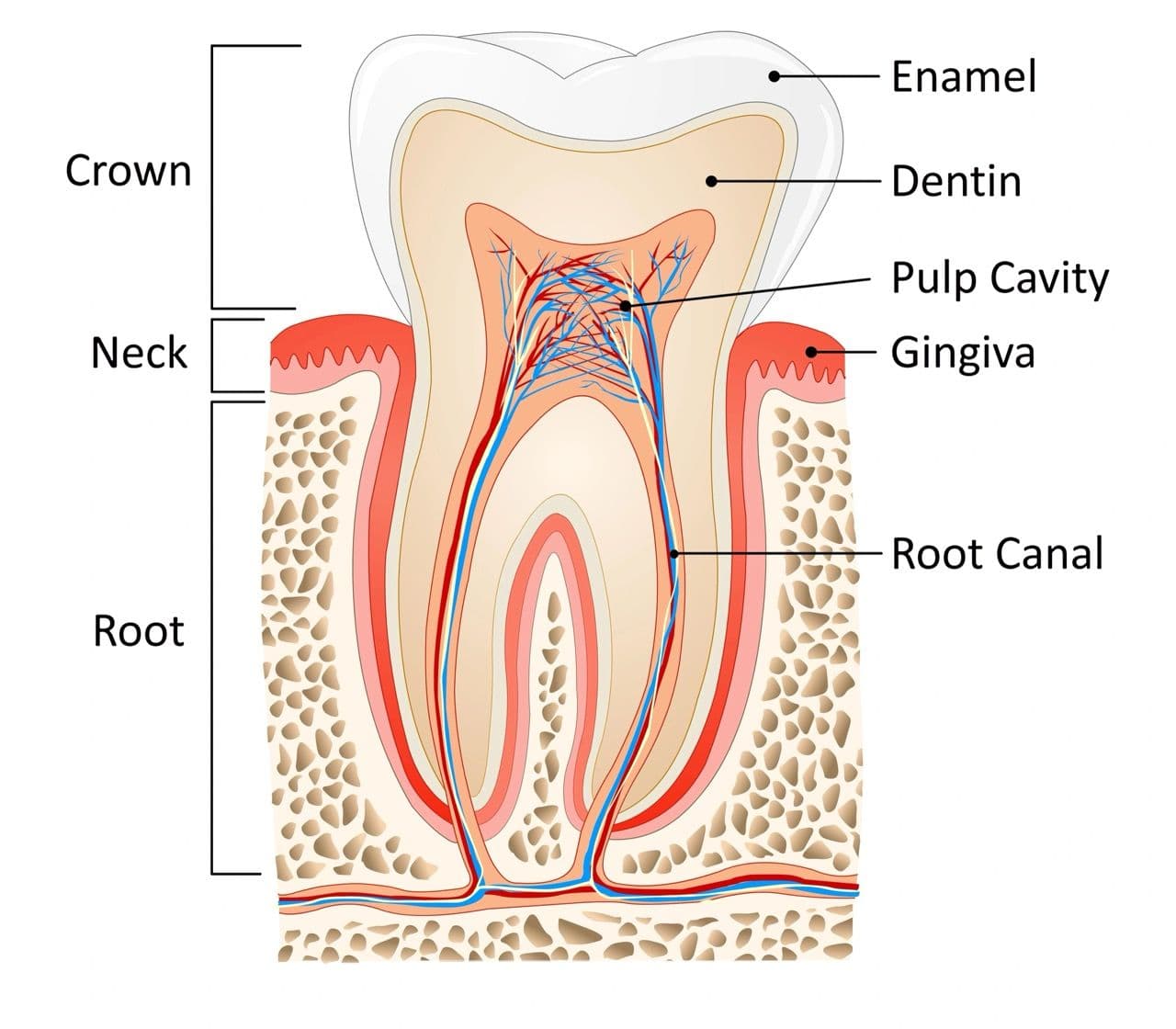
A root canal is a procedure to remove infected or inflamed pulp from inside a tooth. The pulp is the living, soft tissue in the center of a tooth that contains nerves and blood vessels. When bacteria enter the pulp through a deep cavity or crack, the pulp can become infected.
If left untreated, this infection can cause severe pain, swelling or an abscess (a pus-filled boil) at the tooth root. Performing a root canal allows your dentist to clean out the infection, seal the tooth with filling material, and place a crown or filling to protect the tooth. By doing this, the dentist saves your natural tooth, avoiding extraction, and eliminating pain. On average, patients with root canals have a 97% tooth survival rate after ten years.
Common Reasons for Root Canals
You might need a root canal if your tooth’s pulp is infected or severely damaged. Common causes include:
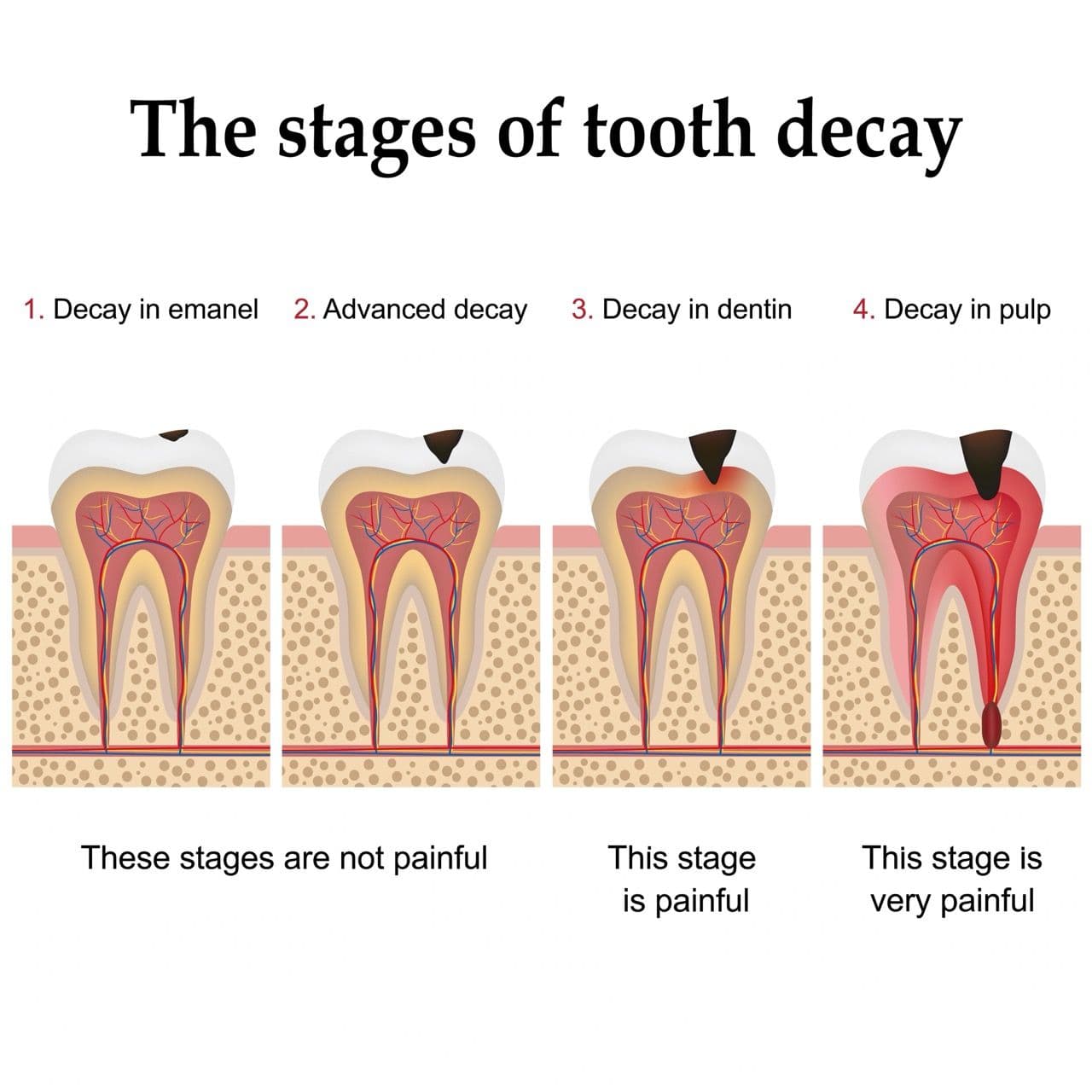
- Deep cavities (tooth decay): When a cavity is untreated and goes very deep, it can reach the pulp and introduce bacteria. Over 20% of adults have at least one untreated cavity.
- Repeated dental work: Multiple fillings or procedures on the same tooth can irritate or weaken the pulp tissue over time.
- Cracked or fractured teeth: A crack can expose the pulp to bacteria, or cause pulp injury even if you don’t see a crack.
- Trauma or injury: A hard blow or accident can damage pulp even if the tooth looks intact, eventually causing pulp inflammation.
If none of these issues is fixed, the infection can spread beyond the tooth. Untreated pulp infection often leads to abscesses and can destroy the bone around the tooth root. Over time you risk losing the tooth or having the infection spread. A root canal stops this process by eliminating the infected tissue and protecting the tooth’s structure.
Symptoms That Signal You May Need One
How do you know if you might need a root canal? Look out for warning signs of pulp infection:
- Persistent toothache: Dull throbbing pain or intense ache, especially if it lasts for days. Pain that comes and goes, or radiates to the ear or jaw, can mean the pulp is inflamed.
- Sensitivity to hot/cold: Lingering pain when you eat or drink something hot or cold, even after the food is gone, suggests nerve tissue damage in the pulp.
- Pain on biting: If biting or chewing hurts, the pulp may be sensitive to pressure. You might feel a sharp jolt or lingering ache when you bite down.
- Swollen or tender gums: Infected teeth can cause nearby gums to swell or become red and tender. You might even see a pus “pimple” (a small boil) on the gum over the affected tooth.
- Tooth discoloration: An infected or dead pulp can cut off blood supply and cause the tooth to turn gray, brown, or dark yellow.
- Loose tooth or swollen face: In advanced cases, the infection can soften the bone around the root so the tooth feels loose, or the jaw may swell visibly.
If you have any of these signs, see your dentist right away. Delaying treatment can lead to serious problems.
How Long Does a Root Canal Take?
In general, plan to spend roughly 1–2 hours at the dentist for a root canal visit. Your dentist needs time for anesthesia, sterilizing equipment, and going step by step through the procedure.
Average Duration by Tooth Type
The length of a root canal appointment varies by tooth. Front teeth (incisors and canines) typically have just one root canal, so they usually take less time. In many cases, a single-canal tooth can be treated in about 30–60 minutes.
However, molars in the back have multiple roots meaning they often have 3-4 canals, making the procedure more complex. Cleaning and filling each canal takes additional time. Expect a molar root canal to take around 90 minutes or more, depending on the tooth’s anatomy. Premolars (bicuspids) are in-between and may have one or two roots, taking roughly 60–90 minutes.
Factors Affecting Time
Several factors can make the procedure take longer:
- Infection severity: If the pulp is heavily infected or there is swelling, the dentist may need extra time to disinfect thoroughly.
- Tooth anatomy: Canals can be narrow, curved, or hidden, which requires more careful cleaning. Molars with complex root systems always take longer than a straightforward front tooth.
- Previous work: Teeth with old root canal attempts or complex restorations may require extra planning and time.
- Patient factors: Patient anxiety or difficulty keeping the mouth open can slow the process. Some patients need extra time for numbing (additional anesthetic) or the dentist to explain steps.
Good communication with your dentist helps. Ask how many canals your tooth has and what the plan is. Experienced endodontists (root canal specialists) are often faster on complex cases, but a general dentist is fully capable of routine canals.
One Visit vs. Multiple Appointments
Some root canals are finished in one appointment, while others may need two visits. This often depends on how severe the infection is and how easily the dentist can clean the canals. For a complex case, you may need to make multiple visits to your dentist, but the majority of root canal treatments are completed within one, two or three visits.
If the infection is mild or a front tooth with one canal, the dentist may clean, fill, and seal the canal all in one session. In this case, you might leave with a temporary or even a permanent filling in place that day.
When there is a severe infection or risk of complications, the dentist might split treatment. In the first visit they will remove the bulk of the infected tissue, clean out the canals, and place an antibacterial medication inside. A temporary filling is then placed. You would return in a week or two, by which time the infection has calmed, to finish cleaning and seal the canals with a permanent filling or core.
With or Without a Crown
After the root canal itself, your tooth usually needs a permanent restoration. In many cases, this is a crown to fully protect the tooth from fracture. Other times, a sturdy filling may suffice.
Placing a crown typically requires at least one additional visit after the root canal. First, the temporary filling is removed and the tooth may be built up or reshaped to hold a crown. An impression is taken and a lab makes the crown (often in a couple of weeks). Then you return for crown placement.
Some teeth (especially small front teeth) may only need a permanent filling instead of a crown if not much structure was lost. In those cases, the dentist will remove the temporary filling and place a final filling in a follow-up visit. Even with a filling, the tooth needs a couple of weeks to fully settle.

Step-by-Step Root Canal Procedure
Below is a simplified walkthrough of what happens before, during, and after the root canal appointment. Knowing these steps can ease anxiety and prepare you for each stage.
Before the Procedure
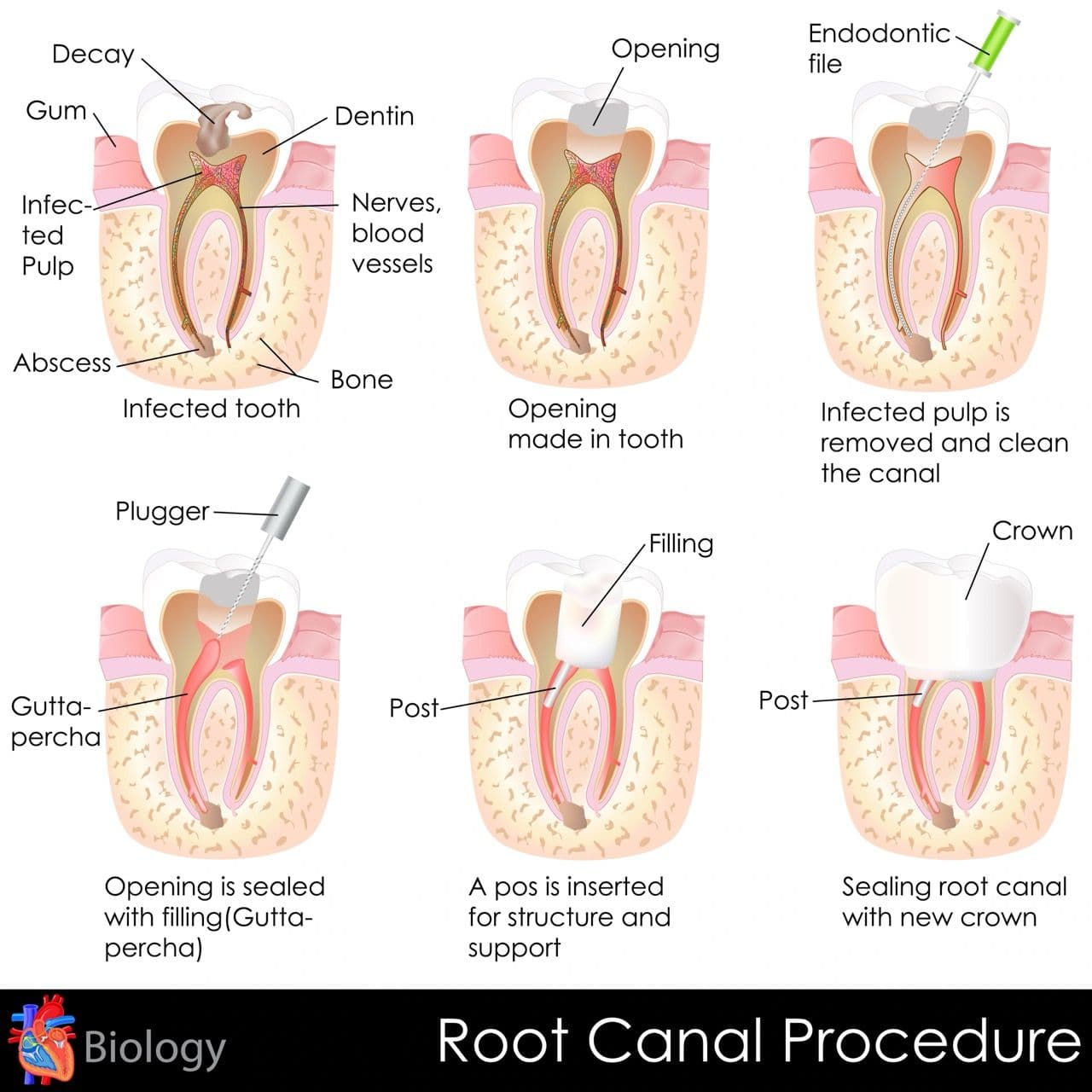
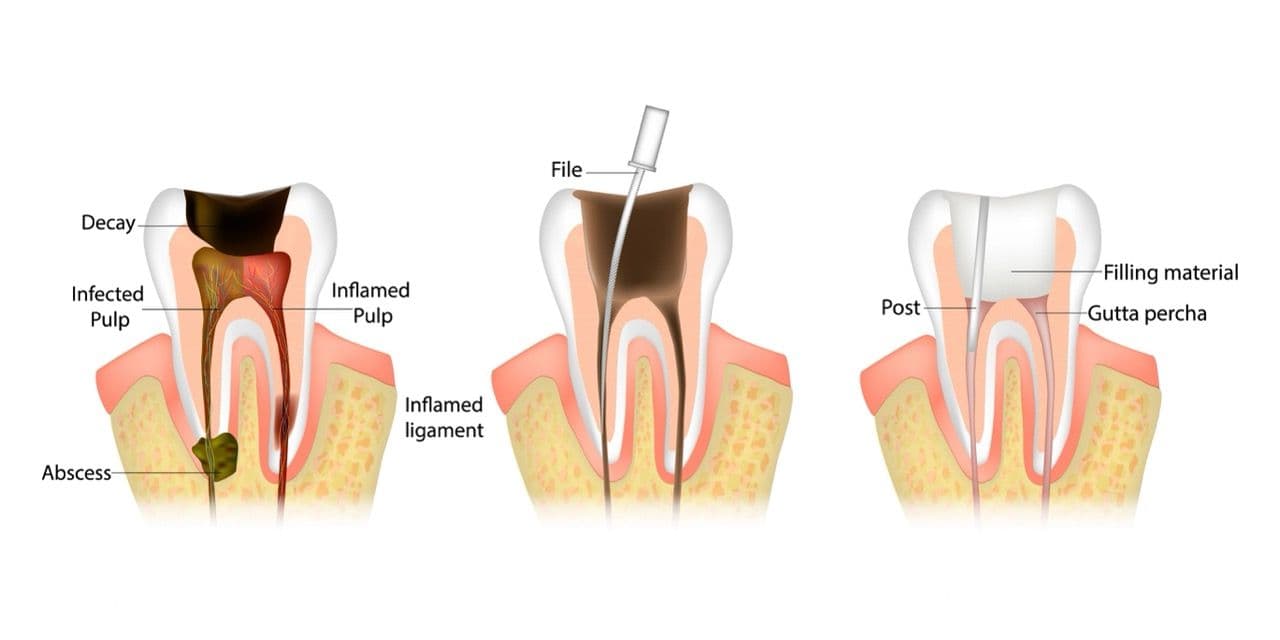
Your dentist will examine the tooth and take X-rays to confirm there is an infection or damage to the pulp. They may tap on the tooth or conduct a ‘cold test’ to pinpoint the problem.
During the Procedure
The dentist numbs the area completely with local anesthesia. You should feel no pain during the procedure. After numbing, the dentist places a rubber dam around the tooth. This keeps the area dry and clean by isolating it from saliva.
The dentist drills a small hole through the top of the tooth to reach the pulp chamber. Through the opening, tiny instruments called files are used to remove the diseased pulp from inside the crown and roots of the tooth. The dentist cleans and reshapes each canal to remove debris and bacteria.
The empty canals are then thoroughly rinsed and disinfected, often with an antibacterial solution. This ensures any microscopic infection is killed.
After cleaning, the dentist fills each canal with a rubber-like material called gutta-percha. Gutta-percha seals the canals and prevents bacteria from re-entering. Cement is used along with it to ensure a tight seal.
Finally, a temporary filling is placed in the access hole to seal the tooth. This keeps the tooth clean until you return for the permanent restoration.
After the Procedure
Once the appointment is done, you may feel numb for a while. It’s normal for the tooth and surrounding gums to feel a bit tender for a few days. Over-the-counter pain relievers like ibuprofen can help manage this discomfort. Swelling is usually minimal but you can reduce it with a cold pack on the cheek if needed.
Avoid chewing directly on that tooth until it’s permanently restored. The temporary filling material is weaker, and biting hard could dislodge it. Stick to soft foods on that side for a few days.
Typically within 1–2 weeks, you’ll return to your dentist. They will remove the temporary filling and place a permanent filling or a crown. If you’re getting a crown, expect one visit to prepare the tooth and take an impression, and a second visit to cement the new crown in place.
Once restored, treat the tooth like any other. Continue good oral hygiene to keep the tooth healthy and attend regular dental check-ups. A tooth treated with a root canal can last a lifetime with proper care.
Are Root Canals Painful?
After a root canal, some mild discomfort is normal as the tissues around the tooth heal. These tissues may have been inflamed, and it takes a few days for that to subside.
Normal Healing vs. Concerning Pain
Most patients report only low-level ache or sensitivity for a short time. Patients may feel some sensitivity for the first few days, which usually responds well to over-the-counter pain relievers.
However, severe or lasting pain is not typical. If you experience intense throbbing, pressure, or if the pain continues beyond a few days, you should call your dentist. Persistent pain could indicate an issue like a missed canal, an undetected fracture, or new infection. In most cases, however, the pain you felt before treatment should be gone after the root canal.
Types of Root Canal Pain Patients Report
People may describe post-root-canal discomfort in various ways:
- Throbbing: A dull ache or slight soreness around the treated tooth for a few days.
- Pain when biting: Your tooth might feel sensitive when you bite down, or your bite might feel a bit uneven.
- Gum or jaw pain: Even though the nerve inside is removed, the ligaments and bone around the tooth were disturbed during treatment. These tissues can still send pain signals until they heal.
These sensations are typically mild and short-lived.
How Long Does Root Canal Pain Last?
Generally, expect the worst of the post-op discomfort to happen in the first 48–72 hours after the procedure. By the end of the first week, most people feel back to normal or only very slightly tender.
- Days 1–2: You may experience some soreness and swelling around the tooth. Take it easy on that side. Ice on the face can help if there’s puffiness.
- Days 3–5: Pain should be diminishing significantly. The tooth may still feel a bit different, but you should be able to eat normally (gently on that side).
- By day 7: If all is well, most patients are pain-free. Any remaining tenderness should be minor. If sharp pain or throbbing continues beyond this point, contact your dentist. This could mean something like a “missed” canal that wasn’t cleaned or another complication.
In summary: mild to moderate discomfort is normal and usually clears in a few days. Severe, worsening, or long-lasting pain is abnormal and means you should go in for a dental check-up.
Pain Management and Recovery Tips
Follow the tips below on how to stop throbbing pain after a root canal. While severe throbbing pain can be a sign of remaining infection, it’s normal to feel some soreness and discomfort during the first week following your procedure.
Home Remedies and Medications
You can manage post-root canal discomfort effectively at home:
- Over-the-counter pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are often the first choice. They reduce both pain and inflammation. Acetaminophen (Tylenol) can also be used if you cannot take NSAIDs.
- Cold compress: If there is swelling, apply an ice pack or cold compress to the cheek for 10–15 minutes on, then off, for the first day. It numbs the area and reduces swelling. (Do not apply ice directly to the skin.)
- Salt-water rinses: Gently rinsing your mouth with warm salt water (½ teaspoon salt in 8 ounces of water) a few times a day can soothe gums and reduce bacteria. Do not swish too forcefully.
- Prescription meds (if given): If your dentist prescribed antibiotics (for example, if the infection was severe or had spread), take them exactly as directed. Finish the full course even if you feel better early.
- Follow the dentist’s instructions: Take any recommended medication as directed. If your dentist prescribed a specific pain medication, use it as directed for the first day or two; you can then transition to OTC meds if needed.
Remember, you should feel some benefit from these measures each day.
Eating and Oral Care Guidelines
How you eat and clean your mouth after a root canal is important for comfort and healing:
- Soft foods: Eat soft, easy-to-chew foods for the first few days. Avoid hard, crunchy, or very chewy foods on that side until you have a permanent restoration.
- Oral hygiene: Continue to brush your teeth twice daily. Be gentle around the treated tooth to avoid irritating the area. Floss carefully near that tooth. You can also use a gentle, alcohol-free antibacterial mouthwash if your dentist recommends it.
- Skip irritants: Avoid extremely hot or cold foods/drinks, very spicy foods, or anything that gave you pain before the root canal. Also, if you smoke, try not to while you’re recovering from a root canal as it can slow healing, reduce blood flow to the area and even increase the risk of infection.
- Follow special instructions: If your dentist gave you any specific post-op instructions (i.e. wearing a night guard if you grind your teeth), be sure to follow them.
When to Contact Your Dentist
While some discomfort is expected, certain signs mean you should get help:
- Pain persists or worsens: If the tooth still hurts a lot after 7–10 days, or if pain suddenly spikes, call your dentist. Lingering pain could indicate that a canal wasn’t fully cleaned or another complication.
- Severe throbbing or pressure: Throbbing pain may mean there is still infected pulp left. This is a reason for prompt follow-up.
- Fever or swelling: Significant swelling of the face, fever, or feeling unwell could signal that the infection hasn’t cleared. Contact your dentist immediately.
- Allergic reactions: If you have hives, rash, or difficulty breathing after taking a prescribed medicine, seek medical help.
- Loose temporary filling: If the temporary filling comes out entirely, keep the area clean with a bit of gauze and arrange to have it resealed.
In most cases, however, following the above care steps will lead to a comfortable recovery.
How Long Does It Take for a Root Canal to Heal?
Root canal recovery is generally quick. By following your dentist’s advice, you should feel mostly healed within a few days to a week.
General Healing Timeline
Within 24–48 hours, most of the numbness and initial soreness fade. By about a week post-treatment, your tooth should no longer be sensitive except in rare cases. Over the course of a few days, the body continues to heal the inflamed bone and ligaments around the tooth.
Remember, the infected nerve tissue is gone, so once the surrounding tissues settle, there should be no ongoing toothache. It’s normal if it takes up to a week for all discomfort to subside.
After the final filling or crown is placed, the tooth is fully restored. There is usually no extra healing time needed beyond waiting for the gum and bone to adapt. If you get a crown, it acts to protect the tooth and allows you to bite normally.
Healing With a Crown vs. No Crown
Because a root canal weakens the structure of the tooth, it’s very common to have a crown placed as part of your procedure. You’ll return after the root canal treatment itself for crown preparation and placement (often 2–3 weeks later). Your dentist will ensure the bite alignment is correct. Once the crown is on, you can use the tooth normally. The additional appointments extend the overall timeline, but the actual healing isn’t different.
Can You Avoid a Root Canal? Prevention Tips
A root canal is often needed when earlier problems have been left unchecked. The good news is you can drastically reduce your risk by taking preventive steps.
Oral Hygiene Habits
Brush twice a day and floss daily. Proper brushing (especially on your back teeth) and flossing prevents plaque buildup and cavities, the #1 cause of pulp infection.
Use fluoride toothpaste. Fluoride strengthens enamel to resist decay. Finally, limit sugary and acidic foods. Cut back on sweets and sodas that fuel cavities. Drink water or rinse after having sugary foods.
Routine Dental Visits
See your dentist every 6 months (or as recommended). A dentist can spot early decay in x-rays before it reaches the pulp. They’ll clean any hardened plaque (tartar) that you might miss at home.
Don’t ignore a small cavity. Filling it promptly is far simpler and cheaper than a root canal later. Once decay gets near the pulp, you’re at high risk for infection. If you play contact sports, use a protective mouthguard. A cracked or damaged tooth is at greater risk of needing a root canal treatment.
What Happens If You Delay Treatment
Delaying a needed root canal can have serious consequences. The infection will not go away on its own and usually only gets worse. Waiting to treat an infected tooth increases the risk that:
- You’ll lose the tooth. The infection can destroy the bone and tooth structure. Eventually the tooth may become unsalvageable.
- Infection spreads. The bacteria can travel from the root tip to infect neighboring teeth or the jawbone. In rare cases it can even spread to other parts of the body, which is a serious health risk.
- An abscess or systemic infection develops. Untreated tooth infections can lead to large abscesses, severe pain, fever, and swelling. These may require emergency treatment or antibiotics. The infected tooth will still need a root canal or extraction.
In short: the earlier you treat an infected tooth, the better. Getting a root canal soon after symptoms start means faster relief, higher success, and less chance of complications.
Scheduling A Root Canal
A root canal may sound scary, but with modern dentistry it’s a routine procedure that can save your tooth and relieve your pain. Today’s root canals are usually quick and comfortable, and most people recover fully in a few days. Remember that early treatment is best. The sooner an infected tooth is treated, the easier the process and the better the outcome.
Don’t let fear or myths hold you back. If you have a persistent toothache, sensitivity, or any signs of infection, contact your dentist today. Affordable Dentures & Implants can explain your options and make sure you get the right care. Early treatment can save your smile and prevent more serious problems down the road.
Schedule a consultation at your local Affordable Dentures & Implants to discuss your concerns and get personalized advice.
Sources:
https://www.aae.org/patients/root-canal-treatment/what-is-a-root-canal/
https://www.cdc.gov/oral-health/data-research/facts-stats/fast-facts-cavities.html
https://www.merckmanuals.com/home/mouth-and-dental-disorders/tooth-disorders/pulpitis
![[object Object]](/_next/image?url=https%3A%2F%2Fcdn.sanity.io%2Fimages%2Fw75voqed%2Fproduction%2F07d4796bc9a2dd89ac0c13de257c139d05469676-4800x3200.jpg&w=3840&q=75)
